High-risk pregnancy | Dr Anu Mahadik Sydney Obstetrician
pregnancy
High-risk pregnancy | Dr Anu Mahadik | Obstetrician Sydney
What is a high risk pregnancy?
High-risk pregnancy | Sydney Obstetrician Dr Anu Mahadik
Who is at more risk of a high-risk pregnancy?
A high-risk pregnancy can result from a medical condition that is present before pregnancy. You are more at risk of a high-risk pregnancy if you:
- Are over 35
- Smoked, drank or used drugs during your pregnancy
- Are carrying multiple fetuses
- Have a history of pregnancy-related hypertension disorders, such as preeclampsia
- Have a history of premature birth
- Have health problems, such as
- High blood pressure
- Heart or blood disorders
- Diabetes
- Obesity
- Epilepsy
- Thyroid disease
- Poorly controlled asthma
- Infections
High-risk pregnancy | Sydney Obstetrician Dr Anu Mahadik
Can you develop a high-risk pregnancy?
Yes, you may not always begin your pregnancy as high risk. A condition may develop during pregnancy that causes your pregnancy to become high risk. Complications can also develop during pregnancy, such as:
- An abnormal placenta position
- Fetal growth restriction (fetal growth less than the 10th percentile for gestational age)
- Rhesus (Rh) sensitization when your immune system is attacking the baby
Twin pregnancy | Sydney Obstetrician Dr Anu Mahadik
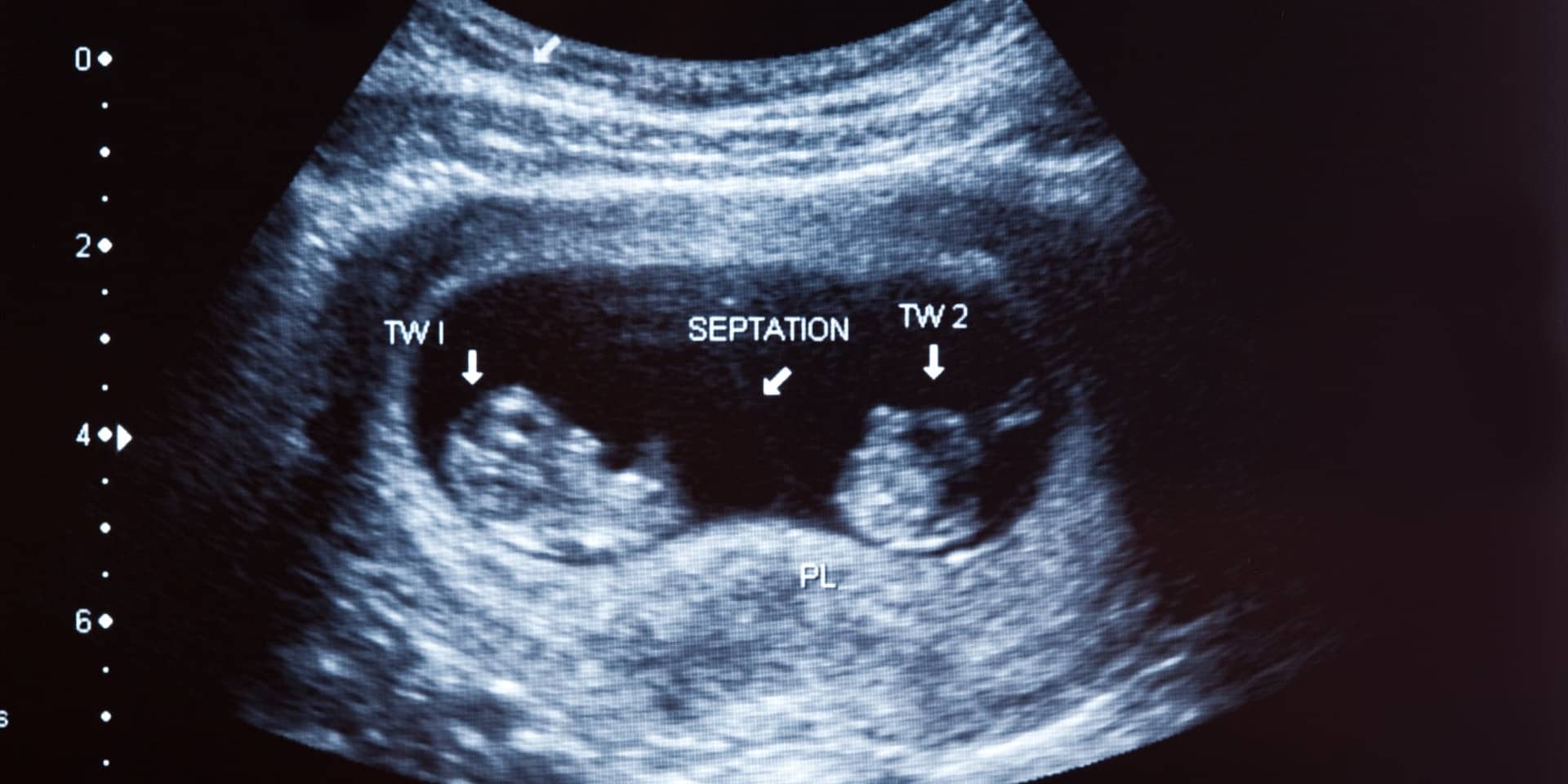
Twin pregnancy
During a multiple pregnancy you can expect more pregnancy related symptoms including nausea & vomiting, heartburn, fatigue, varicose veins.
If you are having twins you will need more frequent checkups. This will be used to track your babies’ growth and development and monitor your own health. You will be watched closely for signs of preterm labour which is more common in multiple births. You may be sent for more frequent ultrasounds and other tests, especially as the pregnancy progresses.
You should be prepared for an earlier delivery. If you don’t then you should expect to have your birth planned before your due date either by an induction of labour or by caesarean section. The timing of birth will depend on the type of twins and any other associated pregnancy complications.
What to do if I’m having twins?
During a multiple pregnancy you can expect more pregnancy related symptoms including nausea & vomiting, heartburn, fatigue, varicose veins.
If you are having twins you will need more frequent checkups. This will be used to track your babies’ growth and development and monitor your own health. You will be watched closely for signs of preterm labour which is more common in multiple births. You may be sent for more frequent ultrasounds and other tests, especially as the pregnancy progresses.
You should be prepared for an earlier delivery. If you don’t then you should expect to have your birth planned before your due date either by an induction of labour or by caesarean section. The timing of birth will depend on the type of twins and any other associated pregnancy complications.
Complications with multiple births
If you are having multiples you need to be aware of the possible complications. This is so you can be prepared and seek medical attention if needed. Just because you are having twins (or more) does not mean you will experience these complications – healthy multiples are born every day.
During pregnancy you have an increased risk of gestational diabetes. An endocrinologist will help you manage your blood sugar levels during pregnancy. You are also more likely to develop high blood pressure. In identical twins, where they are sharing a placenta, a twin-twin transfusion may occur where one baby receives too much blood and the other too little. This is a serious complication and will need to be closely monitored by special ultrasounds performed by specialists.
Twins may be born early. This may result in complications including breathing difficulties, vision problems, infection and jaundice amongst others depending on how early they are born.
Postpartum care of twins
The more babies that you are carrying the more likely you are to have a premature birth and not carry them to term.
If you have signs of preterm labour you would need to be carefully assessed in the hospital and you may need to be admitted and given steroid medications to speed up the development of your babies’ lungs.
This gives them the best chance if they are born early.
Depending on how preterm the labour is, you may need to be transferred to a hospital with adequate nursery support for preterm babies.
Vaginal delivery is still possible for twins. If you go into labour naturally and the first baby is in the correct (head-down) position you may be able to try and deliver vaginally. In some cases you may still need to have the second twin by a C-section if there were complications after the vaginal delivery of the first. If the first twin is not in the correct birthing position a C-section may be recommended. For higher order multiples a C-section is more common.
Depending on whether you have other complications, you may be induced earlier or have a scheduled C-Section during your third trimester.
Hypertension and pregnancy | Sydney Obstetrician Dr Anu Mahadik
Hypertension and pregnancy
Some women may have raised blood pressure during pregnancy. If this occurs after 20 weeks and associated with excess protein in your urine, it may part of complex condition called pre-eclampsia.
Some women have a higher chance of having pre-eclampsia during their pregnancy. These include:
- Women in their first pregnancy
- Women with pre-eclampsia in their last pregnancy
- Women with pre-existing diabetes
- Women with high BP prior to pregnancy
- Women with autoimmune diseases like SLE
- Women with kidney diseases
- Women who are Obese (BMI > 30)
Preeclampsia can affect the placental blood vessels, the effect of which could be:
- Fetal growth restriction
- Reduce fluid around your baby
- Preterm birth and the consequences of prematurity depending on how early the baby is born.
- You will need to be admitted to the hospital
- You will have a drip in your arm
- You will be given medications to lower your blood pressure
- You could be at an increased risk of having seizures and to prevent this you may be commenced on magnesium infusion (given by a drip in your arm)
- Once your blood pressure is controlled, you will need to be delivered (If you are still pregnant)
- You can have severe preeclampsia even after you have delivered your baby for upto a couple of weeks.
- You are at an increased risk of having pre-eclampsia in your future pregnancy
- Taking aspirin in a low dose (started prior to 12 weeks) may reduce the risk of having pre-eclampsia in your next pregnancy. This should be done in consultation with a specialist.
Diabetes and pregnancy | Sydney Obstetrician Dr Anu Mahadik
Diabetes and pregnancy
Women who have pre-existing diabetes can have successful and healthy pregnancies with proper planning and pre-pregnancy counselling.
Pre-pregnancy counselling will allow us to check how well your diabetes is controlled and whether your diabetes is affecting your kidneys/heart/liver/eyes
Ensuring that your blood sugars are well controlled prior to falling pregnant, ensuring that you are on medications safe for pregnancy allow for the pregnancy to have minimal problems for yourself and for your baby.
Apart from optimising your blood sugar control we recommend that you:
- Take folic acid supplements
- Stop smoking/alcohol
- Take immunisations for rubella/chicken pox (if needed)
- Take or change to Medicines suitable for pregnancy
- Regular exercise
Well-controlled diabetes will ensure that you and your baby will have minimal complications from your condition. If your pregnancy is unplanned or if your diabetes is not well controlled, then this can increase risk of complications. This may include:
- Miscarriage
- Fetal anomalies
- Fetal growth problems (growth restriction or macrosomia=big baby)
- Preterm birth
- Stillbirth
- High BP (Pre-eclampsia)
- Increased chance of
- Infections during pregnancy
- Increased risk of needing birth by caesarean section
- Worsening of your diabetes (especially if it involves your eyes/kidneys)
- Ketoacidosis (medical emergency in women with poorly controlled diabetes)
Most babies of women with diabetes in pregnancy whose diabetes is well controlled have an uneventful neonatal course.
However, these babies need to be monitored for:
- Hypoglycaemia
- Jaundice
- Feeding
- Temperature control
If the birth has been difficult and complicated by shoulder dystocia (difficulty in delivery of shoulders after the head has delivered, seen commonly in macrosomic babies of women with diabetes) then the baby will need to assessed for bony/nerve injuries.
High-risk pregnancy | Sydney Obstetrician Dr Anu Mahadik
Fetal growth restriction
What are the causes of fetal growth restriction?
Some babies are small because they are destined to be small, that is they are normal babies. On the other hand, some babies are small because there is either a problem with the baby, placenta or the mother.
The common causes of fetal growth restriction are:
- High blood pressure in mother
- Type II Diabetes
- Long term kidney problems
- Autoimmune conditions such as lupus
- Maternal smoking
- Infections in the baby inside the womb
- Congenital anomalies in the baby
- Chromosomal/genetic problems in the baby
- You will need ore frequent check up’s
- You may be offered further blood tests to look for reasons as to why the baby is measuring small
- Your baby will be closely monitored with ultrasounds
- You may need earlier planned delivery depending on how small the baby is measuring, blood flows to the baby and the fluid around the baby.
Sydney Obstetrician Norwest and St George Private Hospitals
Consulting in Westmead and Kogarah
My consulting rooms are in Westmead. If you are preparing for your antenatal care and looking for the best and most suitable solution, you can count on my practice to help you.
If you live in the Sydney CBD, or south of Sydney, you may be best served by coming to my rooms in Kogarah, at St George Private Hospital Medical Suites.
I am affiliated with Norwest Private Hospital, St George Private Hospital and Westmead Private Hospital.
Westmead Private Hospital welcomes over 2,300 babies into the world each year. They demonstrate a leading and innovative approach to outcome-focused care for women and their families prior to, during and after childbirth.
New parents will enjoy the modern conveniences and perks of a luxury hotel when they experience Westmead Private Hospital’s maternity unit, which has a strong emphasis on assisting new families in the journey of parenthood, with comprehensive postnatal education provided by their maternity team.
They have the unique advantage of being co-located with both Westmead Hospital and Westmead Children’s Hospital. This allows us to provide our patients with the highest standard of private care whilst having access to tertiary level care facilities if required (*access to Neonatal Intensive Care at Westmead Hospital and Westmead Children’s Hospital is dependent on bed availability).
The Maternity Unit comprises:
- 8 birthing suites
- 46 bed antenatal/ post natal unit
- 14 cot Special Care Nursery
- 8 spacious Parenting Suites (additional costs apply)
- Women’s only Infant Feeding Support Centre supported by experienced clinicians
- Education Centre
- Bathing Centre
- Rooftop garden for the whole family to enjoy
- All private rooms with ensuite
Guaranteed Private Room
Westmead Private Hospital is pleased to offer all of our maternity patients the guarantee of a private room following the birth of their baby. One support person is welcome to stay free of charge.
More information on the maternity services at Westmead Private Hospital.
I come from a family of doctors and it has always been my intuitive first choice to become an Obstetrician and Gynaecologist. I basically grew up in it, with my father being one of the co-founders of a series of IVF clinics in India. Care for mothers and the babies they are expecting has always been my first nature and I am grateful for being able to serve my patients in their journey.
So if you are in that phase where you are not sure how to choose a private obstetrician in Sydney, let’s have a chat so we can plan your antenatal care together.